Glaucoma in Singapore
Understanding Glaucoma
Glaucoma is a disease of the optic nerve, the nerve that carries the images we see to the brain.
The optic nerve is made up of a bundle of nerve fibres, and is very similar to an electric cable containing numerous wires. When damage to the optic nerve occurs, patches of blind areas or blind spots occur in a person’s field of vision. In its early stages, such damage to the optic nerve go undetected. In severe or advanced cases, these blind areas coalesce (merge) and visual loss an be profound. If the entire nerve is damaged, blindness occurs.
Once damaged, the optic nerve will not recover i.e the damage is irreversible.
Early detection and treatment are crucial in preventing optic nerve damage and blindness from glaucoma.
Early detection and treatment of eye conditions are key to the optimal preservation of sight.
Schedule an assessment should you experience any eye discomfort or vision problems.
How does glaucoma develop?
In the front portion of the eye, aqueous humour circulates. This is a clear fluid that is constantly produced in the eye to maintain the pressure within the eye. A healthy level of pressure in the eye is necessary to prevent damage to the optic nerve. This pressure is maintained by a dynamic mechanism whereby the small amount of fluid produced is balanced by an equal amount flowing out through the drainage system of the eye.
If the pressure in the eye is such that it increases to a point that is inappropriate for the optic nerve, damage to the nerve fibres occur, and glaucoma develops.
The different types of glaucoma
Open angle glaucoma
This is the commonest form of glaucoma, and the risk of developing this disease increases with age.
With aging, the drainage mechanism of the eye becomes less efficient, and pressure within the eye gradually builds up, causing damage to the optic nerve.
In its early stages, open angle glaucoma has no symptoms, and vision remains normal. As the optic nerve becomes progressively damaged, black patches appear in the visual field. With time, these black areas become larger, and when severe, “tunnel vision” may occur. With total damage of the optic nerve, blindness ensues. Open angle glaucoma is often termed the “thief of sight”. Patients with this form of glaucoma may not know they have glaucoma till advanced damage to the optic nerve occurs.
Closed or Narrow-angle glaucoma
The iris is the coloured part of the eye. When the iris is too close to the drainage angle, it can block the drainage mechanism of the eye such that fluid cannot exit the eye fast enough. Pressure then builds up rapidly inside the eye, causing an acute closed-angle glaucoma attack.
Eyes that are prone to this form of glaucoma are usually small and long-sighted (hyperopic).
Symptoms of an acute closed-angle glaucoma attack include:
- Blurring of vision
- Severe eye pain which usually occurs suddenly
- Red eye
- A headache on the side of the attack
- Nausea and vomiting
- Haloes and glare
An acute angle-closure glaucoma attack is an ocular emergency. Once it occurs, treatment has to be instituted as soon as possible, otherwise permanent damage to the optic nerve and blindness can ensue.
Normo-tension glaucoma
In some cases, the optic nerve becomes sensitive even to eye pressure within the “normal” range, and is at risk of damage.
How is glaucoma detected or diagnosed?
- Regular eye examinations by an ophthalmologist is the best way to detect glaucoma.
- During an eye examination for glaucoma, the following are performed:
- Measurement of the intraocular pressure (tonometry)
- Inspection of the drainage angle of the eye (gonioscopy)
- Examination of the optic nerve (ophthalmoscopy)
- Testing of the peripheral vision of the eye (visual field testing or perimetry)
- In addition, photography of the optic nerve and some other forms of computerized imaging of the optic nerve (optical coherence tomography, Heidelberg retinal tomography etc) may be necessary for some patients.
These tests may need to be repeated on a regular basis to monitor the condition of the optic nerves.
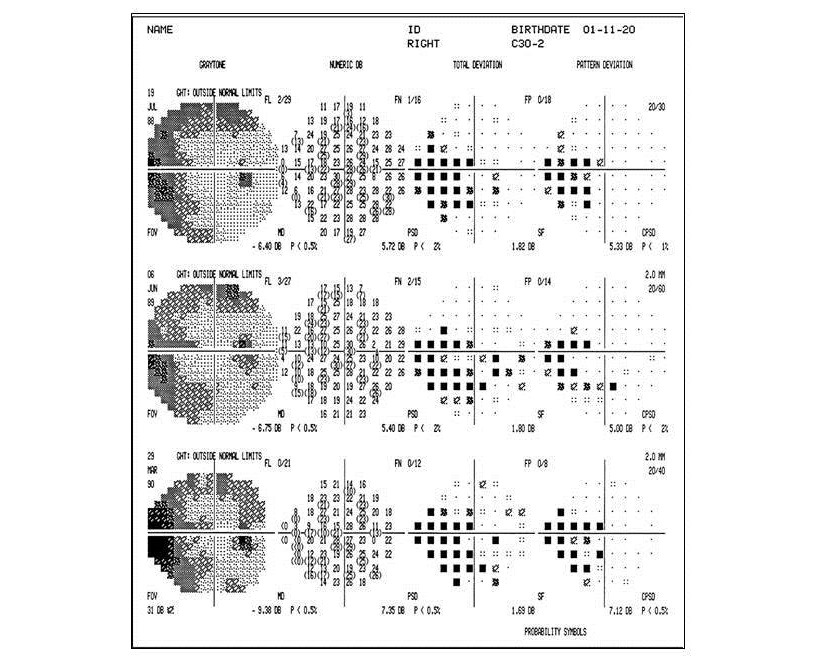
Visual field changes in glaucoma
Patchy areas of visual loss are seen in glaucoma. Termed “scotoma”, these are represented by black squares on automated visual field (perimetry) testing. In advanced glaucoma, these scotoma coalesce, and profound visual loss occurs.
Treatment of glaucoma
Glaucoma is essentially treated by eyedrops and medication, laser treatment and / or surgery.
All about glaucoma medications
Eyedrops
Eyedrops have to be instilled daily. They lower eye pressure either by decreasing the amount of aqueous fluid produced within the eye or by improving the outflow through the drainage angle.
Some of these eyedrops have side-effects, especially when used over the long term. These side effects include stinging, burning, redness, discoloration of the skin surrounding the eyes, changes in pulse and heartbeat, breathlessness (especially in people with asthma or lung disease), dry mouth, change in sense of taste, headaches, blurred vision and change in eye color. However, these side effects are minimal in most patients, and are outweighed by the vision-preserving benefits these eyedrops provide.
Oral medications / Injections
In cases where eyedrops cannot bring down the eye pressure quickly or adequately, oral medications or injections may be required.
Laser surgery for glaucoma
There are various types of laser procedures for glaucoma.
In open-angle glaucoma, drainage is modified by trabeculoplasty. This helps to control the eye pressure.
In closed or narrow-angle glaucoma, the laser creates a hole in the iris (iridotomy) to improve the flow through the drainage system.
Surgery for glaucoma
In advanced cases where despite the use of eyedrops and laser treatment, progressive damage to the optic nerve still occurs, surgery is then indicated.
Your ophthalmologist uses microsurgical instruments to create a new drainage channel for the aqueous fluid to leave the eye. This procedure is called a trabeculectomy. In some cases, special drainage tubes are inserted to improve the outflow of aqueous. These tubes include the Ahmed, Baerveldt and Molteno implants.
More recently micro-stents have been implanted with good results in suitable patients.
The importance of patient co-operation and compliance
Once the diagnosis of glaucoma is made, life-long treatment and follow-up is required. It is important for you to take your medications as prescribed, and make it a point to have your eyes checked every 3 to 6 months as advised by your ophthalmologist. Only then can progression of glaucoma be arrested and blindness prevented.
